Exploring The Distance Between Mental Health Professionals And Neurodivergent People, Pt. 3
Hosted by Amanda Antell. Produced by the Let's Talk! Podcast Collective. Audio editing and transcription by Carrie Cantrell & Chrispy Jones. Web Copy by Nic Meza Honea. Webhosting by Eugene Holden. Visual editing by Ryan Vail and Erik Wideman.
Healthcare, Unafraid.
Article by Nic Meza Honea, Edited by Carrie Cantrell
Meeting a person’s basic needs of food, health, clothing and shelter are essential for a person’s well being.
The subject of this episode is the last in a series of three, delving into the complexities of seeking mental health treatment within the neurodivergent community. Our series emphasizes the need to feel safe and understood in therapy, the importance of practitioners being well-versed in neurodivergent issues, and the impact of negative experiences on seeking treatment.
It is no secret that basic needs are an integral part of mental health, but what are they? Meeting basic needs is measured by some basic principles: having access to food, water, and proper shelter, being in a safe and secure environment for the second part, and being surrounded by loving friends and family. When you have these needs met you are able to leave survival mode and are ready to focus on increasing self-esteem and achieving self-actualization.
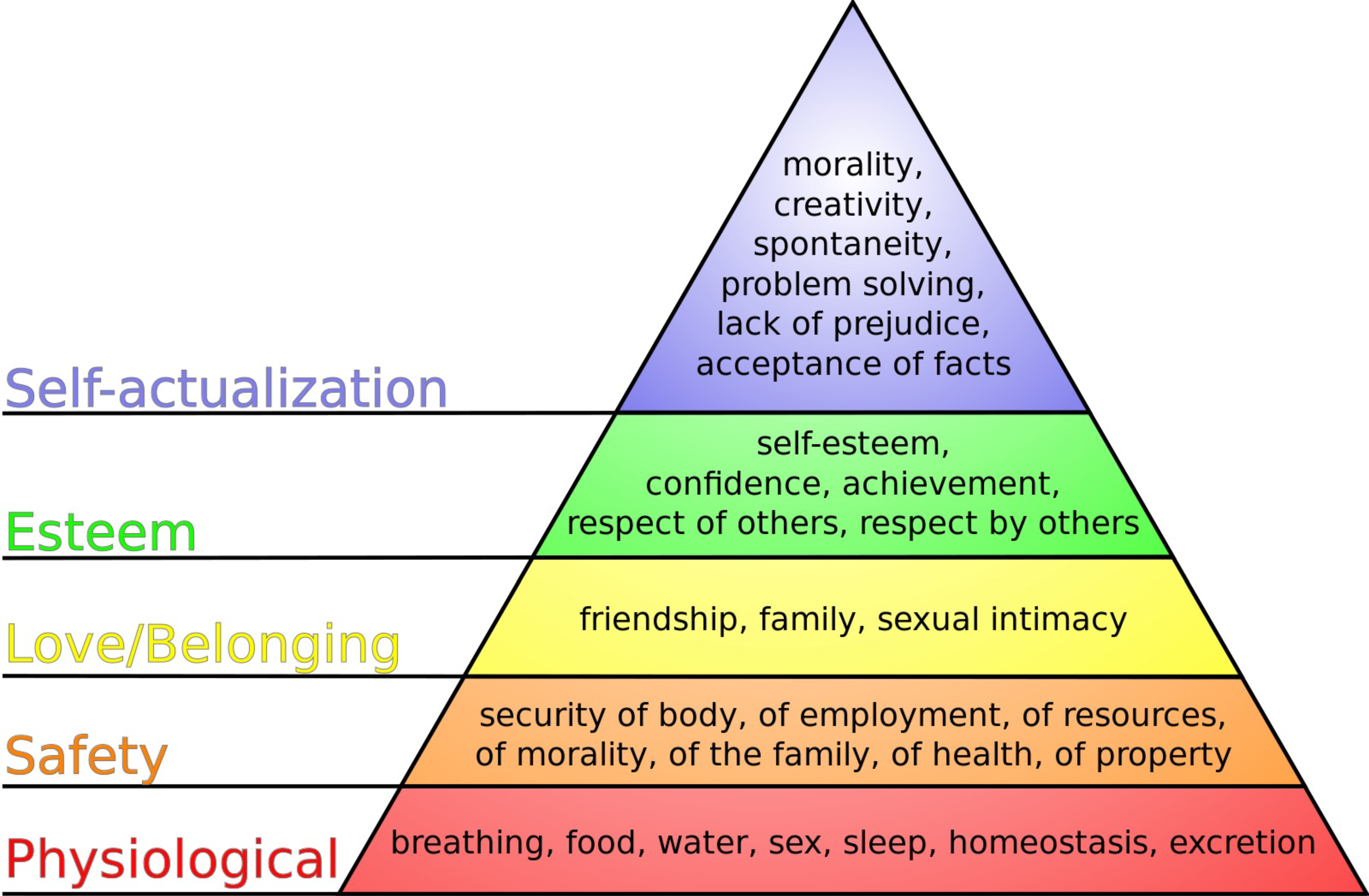
The hierarchy of needs is a concept originating from the Blackfoot tribe, popularized by psychologist Abraham Maslow.
Finding resources can take time and effort. Some folks may not be connected to family and friends, others may be struggling with prioritizing taking care of others like children or elders, and others may simply need to be made aware of what resources are available to them.
While mental health professionals are an important link in your healthcare network, having your basic needs met is vital to the success of your healing journey. Here at PCC, we have some inlets to getting your basic needs met, as well as your mental health healing journey underway.
The community where we are situated in Multnomah County also is able to provide access for residents seeking basic needs and healthcare,
- Multnomah County wraparound for children
- Multnomah County community resources
- Portland government resource page
- Clackamas county basic needs page
- 211 webpage
Many of our students here at PCC are dual enrollees! Here are some pages to connect you with basic needs resources at higher education institutions around the Portland Metro area.
Grassroots organizations are a great resource for people who prefer to avoid accessing resources via institutional structures.
- United way of the Columbia-Willamette Safety Net program
- PDX health and food resources
- Portland Mutual Aid Network
- Mutual Aid PDX – Asset to the Resistance
Community-oriented resources and centers.
- QCenter The largest LGBTQ+ community center in the PNW.
- SMYRC Sexual and Gender Minority Youth Resource Center, serving youth ages 13-24.

SMYRC offers a safe space for queer youth ages 13-24 along with a variety of food, clothing and mental health resources.
- OutsideIn Health care and social services for youth experiencing homelessness and other marginalized people in downtown Portland and the surrounding community.

Started as one of the first free clinics in the US in 1968, Outside In now offers a wide range of services for homeless youth and other marginalized communities.
- Rose Haven A day shelter and community center serving women, children, and gender non-conforming folks.
Named after Portland, The City of Roses, Rose Haven has served as a day shelter for at-risk and homeless women and children since 1997.
- Blanchet House Residential and rehabilitative services for men experiencing homelessness.
- Portland Grief House Community grief support.

Portland Grief House exists to help process grief in many different ways. They have workshops, support groups and one-on-one sessions to help people move through the process of grieving.
- NAYA Native American Youth and Family Center, wrap-around services for the Portland Metro area Native American community.
- Franklin Highschool Resource Center – list of culturally specific resources in Portland, Oregon (main page with general resources).
PDF: Multnomah County Community Resource List H-107, revised 1/2/2019. Credit: Multnomah Co.
Let’s Talk: Autism
Hosted by Amanda Antell
Special Guests: Silver and Carrie Cantrell
This Week’s Episode: Exploring The Distance Between Mental Health Professionals And Neurodivergent People, Pt. 3
New Episodes Every Other Week
Produced by Let’s Talk! Podcast Collective
Exploring the Distance between Mental Health Providers and Neurodivergent Community pt. 3
Transcriptions edited by Carrie Cantrell and Chrispy Jones
Introduction to Let’s Talk Podcast
Erik Wideman: You’re listening to Let’s Talk! Let’s Talk! is a digital space for students at PCC experiencing disabilities to share their perspectives, ideas, and worldviews in an inclusive and accessible environment. The views and opinions expressed in this program are those of the speakers, and do not necessarily reflect the opinions or positions of Portland Community College, PCC Foundation, or XRAY.FM. We broadcast biweekly on our home website, pcc.edu/dca, on Spotify, and on XRAY 91.1 FM and 107.1 FM.
Exploring the Gap: Mental Health and Neurodivergence
Amanda: Welcome to today’s Let’s Talk Autism podcast episode. My name is Amanda, producer, facilitator, and host of this series. We are exploring the gap between mental health professionals and the neurodivergent community. I am joined today by Carrie, Silver, and we spoke on our different takes and experiences with providers. This topic is important not just for autistic people, but the neurodivergent community, because it sheds light onto why so many of us are reluctant or fearful to seek out this kind of care. Even as mental health has become more normalized in wider society, the current treatment plans oftentimes do not work for neurodivergent people. Silver, and Carrie do an amazing job in breaking down the many reasons as to why this might be the case. As you listen to this conversation, I hope you find solidarity in knowing you are not alone in mental health struggles and that it is possible to find the right therapist.
Personal Journeys: Diagnoses and Challenges
Silver: I’m Silver. I use they/ them pronouns. I am majoring in Russian and I’m a stripper and a tattoo artist for work. I have been diagnosed with ADHD. I also definitely have autism and as PTSD count as another condition.
Amanda: I would say so.
Silver: Okay, then that too.
Carrie: It counts. Hi, my name is Carrie Cantrell.
She/her/they pronouns and I am an AAOT transfer student in a communications liberal arts track. CPTSD is my first diagnosis, along with generalized anxiety and being treated for depression. And I’ve undergone a lot of evaluation for ADHD and autism, the process of which kind of broke me, so I’m not able to complete [it], and I know that the process of getting diagnosis requires a lot of family history, which I don’t have a lot of access to. That’s a little bit of my, my background and I don’t have a firm diagnosis except for CPTSD. But yeah, I feel on the Neurodiverse spectrum. We’re a fam.
Amanda: Thank you, Silver, and Carrie. And just, I don’t know, to me, not having an official diagnosis doesn’t exclude you from the autistic community, at least in my opinion. To me, if you, identify as neurodivergent and feel neurodivergent to me, that’s enough. I was diagnosed with autism at age 31. And everyone’s diagnosis, process and journey is different, which will actually relate very heavily to today’s conversation. How long would you say it took you to get either diagnosed and how long has it been since you’ve started your diagnostic journey?
Carrie: Everything for me, diagnostic wise started coming to the surface as I was addressing other health complications as an intersex person, and it’s part of a larger trend of healthcare going untreated in my life, or like not having like acknowledgement of what my healthcare needs are. and so, like the introduction into mental health and understanding my diagnoses kind of came hand in hand, with undoing trauma that had been built up from like years of gaslighting about my identity and circumstances of my youth and stuff like that. So that was in 2015 and I had started going into therapy and other healthcare, for trauma related mental health. Anxiety, having panic attacks and, emotional meltdowns. I like what you called it in one of your last episodes, Amanda, what was it? Like a, a meltdown or something? A shutdown. A shutdown is exactly what it is. And so, it’s been a longer journey to understand about my neurodivergence because for the longest time I regarded the trauma as a permanent wound, and not like a diverse experience that shaped how I perceive the world or how I process information. And so, I was focused on like stopping the pain from that wound or healing that wound, instead of just accepting the diversity of what my understanding of the world is. but then Coming into PCC as a student, there were some resources available to me through accommodations and accessible education, which I needed to access because I was having panic attacks during class and not being able to function with certain stressful situations. And so, opening up that dialogue with my instructors opened up other conversations as well that I was having with my mental health care practitioners at the same time. And yeah, just kind of started talking about ADHD and like I said, went through the evaluation process. It was kind of unfortunate ’cause I got pretty deep into it, but it was as a lot of people experience with state healthcare, I’m on OHP. I was being diagnosed and treated under an academic circumstance, like somebody was treating me and going through my case as a student under tutelage of a professor to get their psychology degree. and so, she and I had a great rapport, and we went very, very far. But unfortunately, it was when she took the information to her supervisor in the academic department that he without talking to me or meeting me at all, kind of like shut down the whole thing because I had disclosed that I imbibe alcohol and I was also on an antidepressant at the time. And so just looking at that piece of information, he said, well, that probably means that, like, that gives her the symptoms of ADHD and she just thinks she has it. So that was extremely triggering for me to put myself in such of a vulnerable situation, to be exposed and to hope for a diagnosis and uncover all of this information. And then just to have someone completely invalidate it, based on two things I use to regulate my central nervous system an antidepressant and alcohol. So, that’s how that diagnostic journey went. I’ve been speaking with my therapist about autism and neurodivergence and he’s entirely supportive. I feel and see a lot of recognition in the neurodivergent community. It’s like so similar to how I felt, like when I came out as an intersex person and I started meeting other intersex people and hearing their stories and I’m like, oh my God, that happened to me too. And so, I have, I have that kind of familiarity with the neurodivergent community and the stories I hear now and the experiences that I’m sharing with other people. So, I’m at the beginning of my diagnostic journey with autism and understanding it, but I’m not in any rush. ‘Cause I hope they don’t come up with a way to. Treat, quote unquote autism or medicate it. Like, who knows? They probably are gonna want to, but I’m not in any rush to get diagnosed because for me, diagnosis, and labels in the medical arena often lead to exploitation. I like understanding myself and understanding what type of supports I can ask for but other than that I don’t trust the medicine industry, which is perfect for this conversation.
Silver: The first things I were diagnosed with was the PTSD and anxiety and depression, and that would’ve been probably in my twenties. The next thing I got diagnosed with was ADHD in 2019. I was also looking for treatment for other stuff, mostly the anxiety and depression. I’ve been, I mean, so the ADHD diagnosis at the time, I was like, huh. And then it was, oh, that makes sense now. I’m still trying to get the autism diagnosis, and state healthcare they were at the point last year, I think when my mom died, you gotta have all your family and stuff involved and I’m already 32 and I was like, well, s**t. People in my family are dying left and right. We better get on this, so everyone doesn’t die before you put that note in my record. That was a year ago and, I don’t know what else to do. A friend of mine said that I should just keep applying for disability so that they can have their own psychologist type person do the assessment on me. cause, even if I were to get a diagnosis from, like state healthcare people, they would not really accept that. But yeah. I am still on my diagnostic journey.
Amanda: Thank you, Carrie, and Silver, it’s honestly okay to still be on a diagnostic journey. It’s like it is what it is. It’s the healthcare system’s fault, not yours. And the fact that you’re actively seeking treatment means that you’re taking care of yourself, and you have really strong self-awareness.
So, for my journey, I was diagnosed with autism at 31, but I should have been diagnosed when I was much younger, like even before kindergarten. But I wasn’t, because I know I’ve said this a million times on podcasts at this point, but autism and ADHD for the longest time were only thought to occur in boys. So, it really was thought that autism was really rare and really rare, and it could only happen in really severe cases in girls during the nineties. So, the result is my mom took me to three different experts and they just did not want to give her an official diagnosis because they didn’t wanna give me a label. And they told her that I would eventually grow out of it. So, my mom just spent most of my childhood trying to make me normal or tried to train me to be normal, then have varying results I think I can navigate neurotypical situations okay, I’m not the best at it, but I definitely can’t really mask very well. I never have been very good at that. So, when I went to see a psychologist at age 31, or psychiatrist, I forget her title to be honest, but it was one of the two. She was actually trained in assessment either way, but. She knew right away I was autistic, but she still just did the three-appointment thing with me because, that was just required. It was just procedure. And she was actually very nice. I can recommend her, at the end of this podcast if both of you want. The problem is she, I, I don’t think she’s under state. Healthcare is the problem, and I’m lucky enough to be in a position where that didn’t affect the process and the way she did it was that she did give me all that paperwork, all the RADS paperwork and everything, but my wife was sufficient to fill it out because my wife A), has known me for a long time but also because she’s a practitioner that believes a lot of stuff regarding autism diagnosis is outdated. Like the whole, you have to have a relative who knew you from when you were three years old kind of thing. It’s like Silver mentioned. A lot of people have a barrier with that because. A), their relatives could be dead or B), they could be estranged, C), they could have like stigmas or prejudices against autism or other mental health conditions, and there could be language barriers or other cultural barriers as well. Point is there’s a lot of issues with that specific requirement. And she also thinks like the RADS toy set was also not necessary for adults because really those are just really used to assess children. So, I acknowledge that there are quite a lot of issues between mental health professionals and the neurodivergent community, which is why we’re having this conversation. But there are some good ones out there. It’s unfortunate that they’re very expensive and they’re very difficult to find.
Carrie: I’ve gotten lucky with a few practitioners in the past, but you’re right, they’re, fewer in between.
Amanda: Yeah. And I know both of you kind of answered number three, at least Carrie did, like, what were the circumstances that led to your diagnosis or what made you seek a diagnosis? But did you want to add anything for question number three to that?
The Struggle with Mental Health Professionals
Carrie: I would say that my experience with mental health professionals specifically has been, actually more toxic up until recently. And, and there’s personal trauma involved with that, but in my opinion, I feel like it’s another level of exploitation sometimes when I go in and asked to be treated and helped by a mental health professional. And I see that you talk about talk therapy and standard therapy like later on., but that’s, that’s one of the things that I feel like is exploitative about therapy is the talk therapy is that it’s almost material that continues someone’s mental health I illness. That’s been my general experience with therapy and mental health practitioners.
Silver: For me, mental health professionals have always been incredibly difficult to find and difficult to get appointments with ’cause like they’re either not taking OHP or Apple Health, the Washington version, or any insurance that, like before I was 26, I could be on my dad’s insurance for work. so, it’s like they’re either not taking the insurance or they’re not taking new appointments or, and then if I do finally get into one, which I think the first therapist I got to see for a long time was in Olympia, and she was more like a social worker, but like, they seem so outta touch. And like, I was living in a trailer in the woods because I moved to Olympia for a tattoo apprenticeship, I was super anxious and depressed, like obviously. But this therapist lady, she was like, why don’t you get a third job? And I’m like, with what time? I’ve got an elderly dog to take care of and I already don’t get paid on this job and I have to drive hundreds of miles every week. And what do you mean just get another job? Do you have any I, which is kind of traumatizing a little bit. It’s like your job is to listen and your job is to like provide support and you’re not doing either of those. And then there’s the waiting list. Like when I moved back to Oregon and got back on OHP here, I was gonna find a therapist and I didn’t get one. I moved back January 2021 and I had signed up for a bunch of waiting lists and didn’t hear back from anyone until like June. And then I got a regular one I think in December and got to talk to her for two sessions and then she quit. And then like January or so, or maybe it was February 2022, I got his third one and they were like, okay, well we don’t know if this one is ever coming back, so we’re just gonna sign you to this guy. And I’m like, how long is he gonna last? But I’ve had this one since then and he seems pretty good. But I’m already 32 and this is a lifetime of not actually getting like respected.
Carrie: I feel like I wanna say that my experience was more that they’re teaching me how to cope rather than to overcome. That’s been my experience with mental health and therapy. Like nobody’s actually trying to see me succeed. They just like saying nice things, when I say sad things. You like your job but, like this is weird for me – that you like your job so much.
Silver: And there’s so much like, oh, we can’t do that for you.
The first therapist I had in Olympia, she, helped me get into housing. Like she goes, oh, section eight is opening up for 75 new applicants on Thursday. And I know that you live in a trailer in the woods with no water, no electricity. And so, you should sign up for this. And I’m like, oh, thanks. And she got in trouble for that.
Carrie: Oh my God. That’s the insane.
Silver: She’s like, don’t tell anyone that I helped you get housing because I’m not allowed to do that. And I’m like, but how can you be a therapist to any, like if their basic needs, like for medication and for food and for housing, if none of those are met, how can you help anybody? Like help them get those things!
Amanda: I don’t know why she would get in trouble. ‘Cause as far as I know, that doesn’t violate anything. But I’m also not a mental health professional, so I really don’t know the guidelines. And also, could just be a Washington policy rather than Oregon. It’s kind of interesting when both of you talk about like exploitative nature of therapy and just the dismissive nature of therapy. I never thought about the exploitative element, to be honest. I’m not saying it’s wrong, but I can definitely see where that comes from. And I’ve heard like a million different horror stories about just how dismissive mental health professionals have been to people in the neurodivergent community. So, I don’t doubt either of your stories for a second. Mom did take me to several different professionals, but they were just evaluating me, so I didn’t really talk to them. And I just remember the only thing I remember about them is that they gave me toy sets and I played with them. That’s it. when I was older though, when I went in middle school, when I was suffering severe bullying and I was kind of becoming more and more despondent to my situation at home, my mom did take me to therapists. The woman who I talked to, she was a nice enough person, I guess, but I felt insulted by her ’cause I just felt like she had treated me like, like I was six. Like she spoke in like this Mickey- Minnie- Mouse voice that drove me nuts. And she just like had over-exaggerated facial expression that she thought was validating, but I just thought was and I just thought she was an idiot. Other therapists I talked to before, the one I have now, I don’t really have anything bad to say about them. I just found them completely useless ’cause they just sat there and just listened to me talk and rant about my life. I just thought that was a complete waste of time and money. So, my experience with therapy has been mediocre, but I did manage to find a good one. And sometimes you just kind of have to follow your gut instinct about what you see online and what you read about online with therapists. And that’s kind of how I found a really good one and she definitely is a lot more affirmative with me. She lets me rant, she lets me cry. She lets me have meltdowns, but she also is very much like, you have to do this, this, and this to get better. And I don’t know, I guess that for me, that works in therapy. I know that doesn’t work for everyone, but that affirmative, blunt stance really does work. So, yeah, that’s been my experience with mental health therapy
Finding Hope and Support in Therapy
Available at the PCC Library. Temple Grandin’s book Animals in Translation explores understanding autism better through the study of animal behavior. Source: Cover courtesy of Harcourt Publishing.
Silver: My favorite therapist ever was the second one I had in Olympia, and she had to quit because of Covid and the scheduling conflicts with childcare, which was a huge bummer. She taught me about EMDR and there was interpersonal conflict stuff that she taught me about that was really eye-opening too. And she believed me with the autism thing and was working with me for the PTSD thing. And it was really sad when she had to quit. She also wrote me a letter for getting two kittens after my dog was dying even though I was already living in Oregon, and she was like, well, my license doesn’t actually apply to Oregon, but let’s try it anyway. Like, I can’t work with you because of legal stuff, but I can try to write this letter because you know these kittens, like your dog is dying. Yes. And you’ve got an opportunity to get more pets and, we’re gonna make this happen for you. I was like, thank you so much.
Amanda: That’s really sweet. Like that, that’s my therapist right there where it’s like, yes, you need, you need kittens for your mental health. My wife was very skeptical for the longest time, and then she saw what those three feral kittens did for me when I brought them into the house, and she genuinely saw like a vast improvement in my mental health.
So, animal therapy actually is a huge thing and I really wish more therapists would implement that because I swear, especially for autistic and ADHD and other, neurodivergent conditions, we connect, at least my experience, I connect with animals a lot better because of the nonverbal aspect and I don’t have to guess what they’re thinking in doing, and that’s actually not unheard of. I don’t know if either of you have heard of Temple. Grandin, but Temple Grandin actually, has a whole book on why autistic people connect with animals better than humans.
Carrie: Really?
Amanda: Yeah.
Carrie: That explains so much. I’ve been obsessed with animals since I was a kid. Animals and nature.
Silver: Same.
Amanda: I have no desire to go camping. I’ll be honest with both of you. I do like hiking, and I do love swimming, so I do like outdoor activities. I hate the actual process of camping though, ’cause of all the work involved, but all the respect in the world, but all the respect in the world to both of you if you like camping.
Carrie: I like glamping. I like being out in nature but like with cushions and blankets.
Silver: and a huge tent.
Carrie: Yeah, a pretty princess tent that looks like something from fantasy.
Amanda: Uh, still too much work, honestly.
Carrie: it is a lot of work, but it’s worth it for like literally 12 hours.
Navigating the Complexities of Mental Health Care
Amanda: So, what are your overall feelings and experiences with mental health professionals treating the autistic, ADHD, and other neurodivergent communities? And does it influence your own interactions and feelings you’ve had with current or previous providers?
Carrie: My overall feelings, experiences with mental health professionals that treat autistic and ADHD and other neurodivergent communities is that they’re gatekeepers.
I have met a couple of excellent practitioners, just like we all have, but we can acknowledge that they’re rare and few and far between people who actually go the extra mile to link you to the thing you’re actually looking for. what infuriates me about the barriers is that like all of these people become practitioners to help. To quote, unquote, help, but like actually end up as gatekeepers, end up as people who prevent access. It’s almost a monopoly on some level that is a part of capitalism unfortunately. That’s been my overall feeling and experience is that people have gone to mental health practitioners about me, and I have had to go to mental health practitioners about myself just to get information that I already recognized was true, but somehow had to be validated by them. Not really sure what’s that about, but…
Silver: I think a lot of them are not helpful and super dismissive and definitely gatekeeping. I think a lot of them are neurotypical also and come from really privileged backgrounds, like how do you even go through this whole program to get your license and do this stuff unless you’ve got like some kind of money and mental capability to function in the society that was built by and for neurotypicals. it makes me not want to like open up to mental healthcare professionals. ‘Cause it’s like, on the one hand, if I say anything, you are probably going to just tell me I am dumb or something. Or making it up or, oh, it’s not really that bad. Like everyone has to drive an hour each way to get to work. You should just get over it and like, that’s not cool.
Carrie: Or they’re gonna blame it on substance abuse.
Silver: Yeah.
Carrie: That’s my favorite is when you go to them with mental health and they’re just like, have you tried not drinking?
Silver: Hate it. And it’s like, well maybe if you had these conditions, you would understand why I need to like drink, right? Or maybe I’ll open up to some mental healthcare professional right away to be I’m so desperate.
And then they’ll be like, oh, well, I quit this job because it’s too hard. It’s like, then I have to like re traumatize myself all the time with all these new professionals. Maybe they’re gonna dismiss me. My favorite was probably, one of the places in Oregon, they were like, on the first Monday of the month, you have to call in at 7:00 AM to ask for being put on the waiting list. And I called in at 7:03 or 7:05 or something and I left a message, and they were like, well, no, you didn’t call early enough. And I’m like, I called at 7:00 AM They’re like, you call at seven oh three. And I’m like, what is the fucking difference? But at least. The one I have now at the place I’ve got, he’s almost as good as the lady in Olympia. And he did get me set up with the grief group in this, institution that helped me through my mom’s death and my best friend’s death. And then also my grandpa’s death last summer. And I was like, oh wow, this is cool. I didn’t think any of this would work. And they also set me up with an ADHD and autism weekly group, which was, uh, a year ago at this time also. And I got a bunch of cool PowerPoints from that. And so, except for them not being able to do the autism diagnosis, the place I’m at now is actually a lot better than the rest of my life experience.
Amanda: It’s very interesting your perspectives. ‘Cause again, I’d never thought about the exploitative element of therapy with neurodivergent communities. And I also never thought about the substance abuse, about using substances against a patient either, because I’ll be honest with you, I’m as square as it gets., I was never around or really exposed to recreational drugs and alcohol. I don’t know. It’s like I tried alcohol here and there when I was 21, but honestly, I hated the taste and because of my autism, the burning sensation was just too overwhelming. So, I never really developed a taste for it. Love my coffee though. I’m not saying my body does not have its vices. And I have nothing against, recreational drugs or anything like that. It’s just… again, I never thought about how it could be used against a patient. So that’s really sad and very interesting because it really ignores a huge aspect of why people might be using, because these substances are often used to numb pain, numb trauma, just so you can get through daily life.
So, if a therapist is using that against you to dismiss you as your overall experience and overall condition as a person, that’s really unprofessional. And quite frankly, I think they should be reported. And I know that doesn’t really sound like it’ll do anything, but I can tell you that it really will scare medical professionals if you report them.
That really will. And I think one or both of you mentioned that family members talk to your therapist about you. And I’m not really sure how this would apply to you as minors, ’cause I think as minors, I don’t remember if parents have access to that information or not. But as adults I can tell you if you don’t give explicit consent to that and your therapist does share that with people, I think the only exception is if it’s like a court ordered mandate or something like that, then you do have right to report them for sharing that confidential information because they are considered practitioners and providers. So just so both of you know that if, you ever feel like your confidentiality was violated as adults, you can definitely report them.
Silver: How does that work for like, I mean, people can get kicked off of services for using any kind of illegal substances, which is a huge bummer. And so, it’s like, maybe we don’t wanna tell ’em if we use LSD or something. ‘Cause they’re gonna be like, oh, well you should kick this person off of housing or food stamps because they’re clearly too irresponsible to deserve it or whatever. And so, it’s like, what if maybe I don’t wanna tell ’em that.
Amanda: Well, you don’t have to but it, so that depends completely on the therapist.
Silver: But I was gonna ask, with the confidentiality thing, like do they get to keep that confidential too?
Amanda: What I would say about that is if it’s a court-ordered mandate, like say you’re arrested for something and you have to show up in court and for whatever reason your mental health kind of comes a part of the conversation, they will be forced to give up that information unfortunately. About the programs, I don’t know a lot about them to be honest with you, but I can tell you that each therapist or practitioner will have like a specific contract with a specific agency or company. So, it really depends on what their contract guidelines are there. And I don’t know if they’re allowed to share that with you or not, honestly. ’cause they have their own NDAs and their own non-disclosure agreements in that aspect as well. I’m not saying that makes the system right and I’m not saying you shouldn’t be wary of that if that is a risk, but if it’s that situation and the therapist is a good therapist, they’re often in a position where they don’t have a choice but to report you.
Silver: It sounds like we should be safe unless something happens to us like legally.
Amanda: I would say that again, if you’re arrested and if your mental health does come into question, there might be a situation where they’re forced to give up their therapy notes about you and just, and even testify against you in court.
Like I know my therapist has that in her agreement.
I’m not saying I think either of you would ever do this, but say if you were on trial for murder, assaults, I don’t know, some other kind of really serious crime. And I think they’re also, I know the medical, providers are required to do this. But if you report any kind of abuse. Then I think they’re legally required to report that as well. I don’t know for therapists, that’s the case, but I do know for doctors and nurses in like other fields in medicine, they’re definitely required to do that and even veterinarians are required to do that as well. That was interesting. You’re in animal health and it’s like, oh, I have to pay attention to the clients as well as the patients. And I’m not a lawyer as well, so I would recommend like seeking actual legal counsel if you’re in a situation like that. Everything I just said, please take it with a grain of salt.
I’m just kind of basing that off of what I’ve read in my user agreement with my therapist and what I remember about it. So, if you’re in a situation like that, I’d recommend just reviewing that confidentiality agreement with your therapist.
Silver: Oh my God, I just remembered one of those stupid agreements in Washington. I told them like I was moving to Oregon and my therapist had quit, but I still needed the medication management from the psychiatrist, and they canceled my last appointment with the psychiatrist that was gonna give me the bridge medication to get me through the first month of Oregon residency again.
And they cancel the appointment. And I was like, Why’d, you do that? And they were like, well, in the agreement that you signed two years ago, uh, you have to be also in therapy. And I’m like, do you remember things you signed two years ago? And they were like, and then they hung up on me or something.
Amanda: So, for that, I’d actually recommend asking for the agreement that you signed because usually non-disclosure agreements do have an expiration date.
Silver: Yeah, I did get my last appointment with the psych and a friend of mine actually came into the phone call with me to advocate for me because I was just like enraged and upset over this whole treatment.
Navigating Mental Health and Therapy: A Personal Journey
Silver: It’s like, yeah, I am moving, but also, we need this appointment. And she made this appointment with me specifically so I could have this, and you guys f****d up.
Amanda: And usually there’s a consent form that you can sign that allows you to transfer to different therapists and that allows it to be okay for the two therapists to communicate with each other. Again, in the state of Oregon, you do have to sign a consent form. I just don’t know about Washington or any other state?
Silver: Yeah, they offered me a new therapist after mine quit, but like she quit in October and I was moving in December and I’m like, I don’t want a new therapist and I’m gonna see twice. And they were like, you said you didn’t want one? I’m like, yeah, ’cause I’m moving. And they’re like, well then you don’t get this. And I’m like, hey guys…
Seeking Legal Advice and Understanding Consent
Amanda: We can continue talking about this if you want, but really, I’m just not a lawyer and I don’t wanna give you bad advice and I don’t want the audience to take bad advice from me either. So overall I would say if you have a question, I would recommend going to a lawyer or like seeking some kind of legal counsel at your university. And usually, a lot of colleges and universities do have some kind of legal advocacy office who actually are a lot more well versed in this stuff than like, say, me. So, they would definitely be a better source of information than say a random person you’re talking to on a podcast.
Exploring the Reluctance of Neurodivergent Individuals Towards Mental Health Professionals
Amanda: This entire kind of conversation we just had goes into the next question about why neurodivergent individuals feel reluctant or even fearful seeking out mental health professionals. Basically, why are neurodivergent people so reluctant to seek mental health therapy even for therapeutic purposes? And the reason I brought up the exploitative element is that I’ve never thought about that I know that it’s a very dismissive attitude mental health professionals have to the neurodivergent communities. I just never have thought about the substance abuse element or the exploitative elements. ‘Cause I obviously have blind spots in a very privileged position.
Carrie: Well, I think we all are, even if we’re just entering healthcare, like in general. But I think that, looking at my history and one of the reasons I’m reluctant to go into mental health is just because of that. Like, I can look at a cost-benefit analysis and I’m like, okay, going into therapy literally causes me this much pain. I to re-traumatize and talk about these things, and also costs me literally this much energy and time out of my day to go and do those. That’s the analysis I have to run in my brain before I do anything, and I think one of, one of the disabilities I have is like a lack of an evocative imagination. Like I can’t picture things, that’s why I feel so stumbly with step-to-step and making progress and looking at an overview of what’s gonna happen. yeah, like I think that leads to some impatience for the therapeutic process and lack of a long term, comprehension of like, how is this actually helping me right now? I have a very literal diagnostic view of how I spend my time and energy throughout the day. I just tend to prioritize other things that have more immediate benefit to me.
The Exploitative Nature of Healthcare and Its Impact on Neurodivergent Communities
Carrie: And then the exploitative measure, well, I think that that feeds into my entire opinion of our healthcare industry in America. It just makes me so angry that first of all, that there is a conflagration or a conflagration or whatever of having a disability or having neurodivergence with illness. Disability is a diversity and it’s a unique experience as you move through life. It’s a body shape, it’s a perspective, it’s a processing. So that’s one thing that feels exploitative to me is treating people who are natural and diverse, just in a world that’s not meant for them, not built for them. Is exploitative, just on a fundamental level. Like, okay, well since we made up this like really square world of right angles and boxes, and you happen to be a roly-poly, we’re just gonna treat being roly-poly as if it’s an illness. You know what I mean? And so that’s the exploitative part, it comes from capitalism where there’s like literally an entire industry, like, so many levels to the factory floor, I guess, I don’t know. It’s like treating people like they’re products to be, consumed or processed. And that’s what happens to neurodivergent communities. That’s what happens to disabled communities, and that’s what happens to marginalized communities in general.
And there, there is such a thing as like toxic advocacy. There is such a thing as like toxic medicine. There is such a thing as toxic community. And I think that’s like kind of part of it, when somebody situates themselves as the gatekeeper, the savior to your experience. that’s the exploitative nature. And that pretty much just describes our healthcare industry in general. And mental healthcare is just part of that.
Silver: I think that leads into like eugenics and stuff, ’cause once you’ve got into this process, what if maybe the far right takes over and now, you’ve got records that you’re, neurodivergent and disabled. And then the, the, the right-wing people are like, well, we don’t need you, you don’t need to be alive.
The Fear of Historical Medical Practices and Seeking Safety
Silver: Like, I was really afraid of going to get any kind of mental health. When I was in my twenties, ’cause I didn’t want the Nazis to kill me. And like I was taking German in high school. Like I was really into German history and I’m like, oh my God, I don’t want to be murdered by these people so I would better, I’d better just hide and pretend that I’m normal, even though it was like painful. And then I was like, I don’t actually wanna pretend that I’m normal, but as long as I’m not disabled, then the Nazis can’t kill me. And then there’s like the infantilization, it’s like, oh, well you’re ADHD or autistic or traumatized or whatever. Well, you, you obviously need someone to help you and you can’t make decisions for yourself and so we’re gonna make them for you. Like, no, I don’t want that. I don’t want that at all. Like lobotomies, like we don’t want the treatment for autism to be a lobotomy. It’s, it’s like, like as if it were 1950 all over again, like having respect from the medical institution would be great. Having respect from other people would be great.
Carrie: It’s easy to say it sounds paranoid, but then I think about literally last generation, my grandma’s generation lobotomies still happened on a regular basis. So, it does still happen. And this is what happens when we put, our humanity in the hands of an institution. And that’s what neurodivergent people are asked to do when they go into mental health care and ask for validation.
Amanda: Very interesting perspectives. I’ll be honest, like the way I look at mental health institutions in America is that you have two sides of it. You have people who go in it for the money and the exploitative nature. Most definitely. But you also have people who do genuinely want to help people. They just really don’t know how to do it because they were not trained by neurodivergent people. So, they approach it from the neurotypical level. And as much as I like my therapist, there have been times where I’ve really had to kind of get her to listen to me and turn it back around on her. Like I was dealing with someone who doesn’t even have any mental health training and they’re essentially typecasting people with ADHD. And I had to explain to my therapist why that was so bad by turning it around on her and say, how would you feel if I dismissed your health issue that you disclosed to me? Because my perspective would be I’m doing you a favor by forcing you to be more normal. When you turn it around on them, they kind of realize just how bad that is. And it’s interesting that they don’t ever really think about that before that. And I feel like neurodivergent people, to me, are actively thinking about that, how they’re feeling and how they might make someone else feel. At least to me, the three of us kind of strike me as that. So, Silver’s comments about the eugenics aspect. I don’t think I’ve ever been that paranoid about it. I’m not saying that your feelings aren’t invalid, certainly, but for me, I’m just thinking about how the lobotomies and the electroshock therapies really just stopped with autistic people really recently, and I know I’ve mentioned this organization before, but Autism Speaks is basically like the world’s biggest and most successful hate group against autistic people.nd they supported a program for the longest time that tried to cure autism, quote unquote, through electroshock therapy. And I know that originally, they were like subscribing to lobotomies for autistic people. So no, I don’t blame both of you for being really wary of mental health professionals like that is very valid and that’s why we need to have this conversation. Because the mental health professionals need to hear our fears, our concerns, and why they need to make more effort to actually talk to us and at least try to understand where we’re coming from with our distrust.
Challenging Traditional Therapy: Neurodivergent Perspectives
Amanda: And Carrie, your kind of mentioned talk therapy earlier and do you mean like standard therapy?
Carrie: Yeah, I think, like standard talk therapy where you sit down on a couch, or a chair and you basically are allowed to just vent on some situations. And other times you have more exploratory conversations about feelings and trauma and memories and stuff like that and, interpretations. For me that has never been fruitful. it’s never been a good outcome, I’d say. not in building relationship with a therapist that I believed could help me or building a relationship with myself., I think it’s kind of just dragged a lot of stuff on. But on a more positive note, I would say that I recently have begun didactic behavioral therapy, which is offshoot of CBT Cognitive Behavioral Therapy. and I’m also starting group sessions as well, which is something new for me. It’s a new tool to go through this as a group and as a society because like isolation and social communication is something that like, it’s really difficult for me, I mean, I’m a talker obviously, with people I trust, but like the anxiety is real. So yeah, I’d say traditional or standard therapy doesn’t necessarily work. I’d say it would at least be appropriate to ask for a specialization, somebody who has, a lot of experience with neurodivergent communities or is perhaps neurodivergent themselves, which is the case with my current therapist.
Silver: Yeah, I was thinking about that question because last year in my group that I was in, they were talking about how standard psychotherapy is mostly like a top-down approach and for ADHD and autistic people they do better with a bottom-up approach. And when that was brought up, I was like, I don’t understand, but like I opened the slide. It says that the bottom-up thing is like body sensory, what’s going on? And remember that we can only really focus on a couple at a time. And then the stimming behaviors starting with what’s going on physically and then going up into brain stuff and psych normal therapies are like brain stuff, which then is supposed to control your body stuff. I haven’t had an opportunity to see whether or not either of those work. I guess since I don’t really know what regular therapy does, even though I’ve had a therapist for a while. But it, like, it makes sense because if I am having a lot of experiences in my body, I can’t really brain any at all. So like, how am I supposed to make choices on what’s important to put my attention onto, cognitively when so many things are happening physically? Also, they brought up that the CBT is more effective with children than with adults, but I, I also don’t really have experience with that either.
Amanda: so, I think the idea of top to bottom therapy, kind of like you mentioned, I think the idea is you’re just kind of getting to know someone slowly and gaining their trust slowly, I think is the logic behind that approach. But I do agree that it ignores the fact that autistic and ADHD and other neurodivergent conditions feel sensations very strongly. we actually feel physical sensations with our emotions very strongly. Like when I get angry and stressed and on the verge of a meltdown, my body temperature rises, my heart rate goes up. My respiration rate increases obviously. It’s like when we feel those physical aspects, and they’re ignored, that becomes a lot harder for us to process. And it just is gonna make the whole process longer and more traumatizing to open up.
Silver: This slide also says, research for adults is like, mindfulness helps us being able to recognize what’s going on in our bodies. First step to being able to do anything to regulate what’s going on in our bodies. It’s as, I mean it then it’s a sleep hygiene, nutrition, and exercise. If I haven’t slept, then I’m gonna be dysregulated and I’m not gonna be able to do any brain stuff. And if I haven’t eaten then I’m gonna be dysregulated. I’m not gonna be able to do any brain stuff and exercise helps me be able to do brain stuff.
Amanda: Yeah, that checks out physiologically.
Carrie: I can’t function without exercise either.
Amanda: For me it’s sleep. Like I have a sleep disorder called delayed sleep syndrome, where my body literally does not even produce melatonin until like three A.M. So, I actually take sleep supplements for sleep. When I got veterinary shadow hours, the early hours, like when clinics would open at eight or nine would just kill me because it’s like, oh my God, I wanna be a veterinarian one day. How am I gonna perform surgery when I’m half dead? And then I discovered emergency, and I was really happy ’cause I can be awake at midnight and perform surgery and be the Energizer Bunny and be like, yes. I loved it and I, yeah, I loved emergency. Miss it. I miss it. But anyways, so I do get the whole dysregulation with sleep because it’s like, as weird as my sleep schedule is, I do need it to function. I can go a long time without eating. Interestingly, I don’t like to do that, but when I get stressed and just overworked, I just forget to. My wife gets annoyed with me about that. ‘Cause she worries about my health when that happens. As she should. And yeah, the whole physical body wellness thing definitely is important to us. I really wish I had paid attention to the nutritional aspect when I was younger though. I do now, but it’s really horrifying to think what I ate when I was younger after taking a lot of biochemistry, anatomy and physiology classes like that will ruin your perception of health. I will warn you, if you take a lot of those classes. So, going to number seven, do you think that the mental health professional community, like the American Psychological Association is well versed in neurodivergent issues? Why or why not? And I think we can all agree no, but even if this is an obvious question, it’s about saying it out loud, that kind of sheds light on it.
Silver: Yeah. It seems like they aren’t well versed enough. I think it’s because there aren’t enough neurodivergent people involved. It’s just a bunch of neurotypicals thinking that they know what’s best for everybody.
Carrie: Yeah, I would say that. I mean, even just doing searches on their website it’s still very clinical and I don’t think there’s a whole lot there. There is definitely like cited articles that you can go and research, but like, maybe you can elaborate. What would being well versed on autism mean?
Amanda: For me, it’s like just not making all these assumptions about what, what works for us when it works for like neurotypical people. I feel like that’s a huge weakness in my own experience with mental health professionals. It’s just these blanket recommendations of just try something. Just do this, just do that. And I did mention that my therapist does kind of do that. But she only makes suggestions like that after talking with me at length about an issue. She just doesn’t automatically get impatient with me and just say, just do this or just do that. ‘Cause there’s a lot of barriers and anxiety in and of itself in some situations where you’re like really reluctant to try something. Like for me, trying to think of a good example for me, for me it was just those feral kittens that I had mentioned before. I had so much panic and anxiety when they were outside because it was the dead of winter, and I was worried that literally anything would kill them. Like a rat or a raccoon, a coyote. ‘Cause they were just so little, and they had a good mother and everything. But I lost so much sleep and I’m pretty sure I aged 10 years with that whole process, catching them. And my therapist just had to kind of teach me breathing techniques and just regulate myself during that whole thing just because it was just such a stressful situation for me. Eventually I finally did have to take action and finally catch the mom and the babies after making remote triggers with my father-in-Law. That was actually really cool to learn engineering skills for that though. So, it’s like just looking at us as individuals and not as like part of like general society. We can’t treat us as neurotypical people. We just don’t process things the same way. At least that’s my 2 cents on it.
Carrie: I would say the approach is like to they treat society rather than treating us. You know? like all the treatments are centered on us accommodating society or expectations and kind of like the standard of practice, right? to teach coping, but not, uplifting, or spontaneous creation or incubation of your own goals. That’s kind of my impression of psychological standards and all of this is that like, okay, it’s so that we can be seen as acceptable.
Amanda: So, it is kind of like treating society as Carrie said, but it also kind of goes back to what I’ve said in previous podcasts where therapists or mental health professionals, everyone around us, I feel like kind of does this to us, where they think they’re doing us a favor by forcing us to be normal, whatever normal even means.
I really do think that’s a huge element with mental health professionals where they are trained to think they’re doing us a favor by making us be like everyone else essentially.
And just kind of integrating us into society.
Silver: I’m just like, uh, that’s so dumb. And I hate it. And I wish that it was different. Like, they should be treating society in the way that like, makes society more accepting of multiple different ways of being. Like there isn’t just, I.
There’s no such thing as one size fits all. It’s, it’s just like we’re not all the same person and we should embrace the fact that we’re not all the same person and that all of us need like different things like forcing us all to be day people. Why? That’s so backwards. Or forcing us all to be type-A personalities or forcing us all to be extroverted or forcing us all to be parents or something like, no, there’s good reason to embrace and respect folks who are different and, when I was looking into doing the vet tech thing too, people are like, well, Silver, you’re not a day person. What are you gonna do if you go through the vet program? Like, well there’s like nighttime stuff and there’s zoos and there’s emergency. So like, I don’t have to be a day person.
Amanda: So much that. Again, I, I felt at home with emergency ’cause of a constant stream of like stimulation too. So, for number eight, this is actually kind of an important one.
The Importance of Understanding and Compassion in Therapy
Amanda: As a neurodivergent community member, what do you need for mental health professionals when seeking treatment and have these needs ever been met?
Carrie: Well, number one, I need to feel safe in an environment, right? As an already triggerable and hypersensitive person, being understood for the sensitive aspects, like the literal sensitivities I have, is helpful. Some things seem louder or more intrusive to me just because it’s hurtful as a sensation that’s unique to my experience. So that’s just number one, understanding that when I’m in treatment, it’s also a multiprocessing level. Like it’s not just talking about whatever I’m there to talk about. It’s also processing the information that may or may not be excruciating or displeasing in some way besides just being traumatic. It could be like a tactile sensation that’s really distracting me. It could be a sound frequency that’s really reverberating my eardrum and making wop, wop, wop in my head right now. And it could be intrusive thoughts. And so just having that understanding is good. And it usually takes a couple of sessions for people to understand that like, okay, Carrie has like some sensitivities about some things, but then after that I think that the biggest need that is sometimes met, is compassion and consistency. I think maybe that sensation of rejection is something I’m also really, really sensitive to and hyper vigilant of, just because of past experiences. And these needs, they have been met. Like I said, I’m currently working with a therapist and they’re also neurodivergent, so they’ve got the compassion and the understanding, and we’ve had some very frank statements. Yes, literal declarations of what’s happening and what the needs are, and it’s like so helpful sometimes to just talk literally and not have it be taken personally. It’s wonderful. So yeah, thank you for asking that question. It’s a good one.
Silver: Definitely. Needing to feel safe in a medical setting where like they kind of have your life in their hand is so important. And part of that is also like respect. if they listen and then pretend that they agree or understand or whatever, but it’s obvious in their actions or their response that they don’t, it’s like, what are, what am I here for? And no gas lighting and no infantilization and no, platitudes or something
Carrie: I’m just gonna call it like no spectating either. Like, I’m not here to be a freak show for you.
Amanda: but it’s like, before I get too off track I just wanna say that what I need from a mental health therapist is do not try to make me normal. Do not try to integrate me in society, listen to me and what my needs are so I can function in society so I can win in society. Again, I’m not, I’m not a mountain climber, but I just have seen videos where people are like scaling ice walls with those pickaxe things. I’m probably gonna get destroyed for using the wrong mountain climbing equipment terminology, but, oh well. Mm-hmm. I can, I just shouldn’t have to do that. So that’s what I would say is that I think my perspective is yes, I’m a customer, but that also means that they have to kind of make me happy.
So, if I’m not happy with them on some level, I can report them. I try not to be a Karen, but it’s like if I feel like I’m disrespected or not treated well, I do kind of go back and look at what they did and I’m like, okay. Let’s see how we can improve the situation. And I’m not really necessarily even looking to get someone fired, it’s just that I want them to be aware of how they treated me and how that might affect other people. That’s kind of my goal with that.
Advice for Neurodivergent Individuals Seeking Therapy
Amanda: So, what advice would you or Silver have to other neurodivergent community members seeking therapy?
My advice is trust your gut. Like that’s really been my strategy this whole time with therapy. And if you don’t click with someone regardless of what the reason is, you don’t need to feel bad about dropping them as a therapist and finding someone else. You need to find healthcare professionals that, as both of you have said, feel comfortable and feel safe enough with, and sometimes that really is just clicking with their personality. It really does come down to that. ‘Cause if you click with them, you’re going to, you’re automatically gonna be more comfortable around them. You’re automatically going to be, I’m not saying it’s gonna be a perfect relationship because obviously you don’t know each other and it’s gonna be a process for both of you. But you have to actually feel comfortable with someone to do that. So don’t feel bad if you have like really bad gut reactions to therapists that you book with, even if you wait months out some. ‘Cause here’s the thing about therapy. One bad therapy session is going to taint your entire idea of what therapy is. And versus like, if you have consistently good ones, you’ll be less reluctant and you’ll have at least less traumatizing experiences to, to look back on, to, to suffer through, to go through. Like I mentioned, those therapists in my childhood where I didn’t hate them, I didn’t dislike them and I wasn’t abused by them or anything, but I didn’t click with them, and I honestly thought they were a waste of time. So, I’m not sure if that helps either of you, but that, that would be my advice to people in the neurodivergent community. Trust your gut and don’t feel bad about it.
Silver: Mm-Hmm. Yeah. And I would say keep calling around. Get on the waiting lists. Like maybe you don’t have the spoons to do it this week, but like next week. ‘Cause it’s, you’re not gonna find one you click with if you don’t call around.
Carrie: I’d say my only piece of advice is to talk about your experiences. Because I think a lot of us don’t know what to expect or what the standards should be, especially when we’re in a state seeking, seeking care and seeking security and like maybe we don’t know what to look for in healthy relationships in therapy relationships and stuff like that. So, I would say yeah, like seeking recommendations and talking about it with peers and other neurodivergent people to see what has worked for them. Because I, I bet like you probably at least have a more initial, if you have had negative experiences with mental health in the past, my guess is that you would most likely have a more trusting relationship with your peers than you would with another type of referral service. So yeah, touch your community and don’t put all of your faith into the institutions, just being around people who help you feel normal or at least not monstrous for how you are and how you don’t fit into, a typical society does wonders for your mental health. And it’s not that there’s anything wrong with you that needs to be solved, it’s that you’re under distress because like. The pressures of not, not fitting in and not being able to plug in to, to a society that has not been shaped for your needs. So, I think building a society, a new society and surrounding yourself with people who understand those needs and accept them and accept your diversities is one of the biggest keys to mental health and also the best resource ever for finding the best doctor.
Amanda: Yeah, and I also had some other thoughts that came to mind as you were talking. Be aware that yes, it is kind of a difference in power where the professional does have more power than you technically, but you’re also the customer and it’s actually a lot more equal than you realize. So, if they do something to make you feel uncomfortable, and if you think that they were just unprofessional with you, don’t feel bad to drop them and even report them again if they make you feel that you have. So, I just want people in this, the audience to be aware that they do have rights as a patient and that they def and that they definitely are owed decent and empathetic care.
So, are there any final questions or comments you have?
Reflecting on the Mental Health Journey and Advocating for Better Care
Carrie: I do have a very dubious opinion of a lot of mental health practices. And I think I spoke a lot about some negative experiences, and I spoke about some positive experiences I’ve had as well. But I wanna say, ultimately making the decision to discover mental health and work on it and treat it, even though it hasn’t been an extremely linear, easy, straightforward journey has been worthwhile. Like the obstructions, the doofus doctors, like all of it is holistically part of what you’re going through.
And some of that journey will suck. But, ultimately looking back over the last, like however many years it’s been since I started that journey, I am in a better place than when I started. So, if anybody is thinking about seeking mental healthcare and you’ve been struggling and it’s not an experience you’ve had before, I wholly would recommend it.
And just be ready. Entering mental health care isn’t like a magic pill that fixes everything. There’s gonna be the exact same bulls**t on the inside of that therapist’s room as there is on the outside of the world. But like, the difference is, is that you’ve got somebody across the room from you who is literally being paid to help you find solutions. That switch in attitude is, is the biggest thing in changing my life. That’s how I try and understand it, is that even if it’s not perfect in the moment, the big picture baby.
Silver: I wish that we could just make universal basic healthcare a thing so that there are less hoops to jump through. These hoops get in the way. They’re, they make it so much harder. It’s unnecessarily difficult and it’s unnecessarily traumatizing sometimes too.
Amanda: Thank you very much Silver and Carrie, like this conversation was very enlightening and it definitely gives me more thoughts about the mental health profession and how it’s kind of just overall impacts the neurodivergent community.
Closing Thoughts and the Mission of Let’s Talk Autism
Amanda: Thank you for listening to today’s Let’s Talk Autism podcast episode. As you just heard, there are many reasons why neurodivergent people either choose to abstain or are very reluctant to seek mental health treatment. However, the main takeaway I want the audience to have been that the general distrust and negativity surrounding mental health professionals in our community stems from years of dismissal, misinformation, abuse, and exploitation. As mentioned, standard talk therapy doesn’t always work because it ignores the physical sensations neurodivergent people feel at a given time, and it doesn’t take into account other outside factors. I want the audience to know that they have rights as patients and are under no obligation to stay with a practitioner they don’t feel comfortable with and have the right to report them for misconduct. Ultimately, a mental health professional is duty bound to provide you with a safe environment in which you can talk and recover at your own pace. They are not entitled to your money or time if the service is not met. Thank you for listening, and I hope you tune in for the next episode.
Erik Wideman: Thank you for listening to Let’s Talk, Portland Community College’s broadcast about disability culture. Find more information and resources concerning this episode and others at pcc.edu/dca. This episode was produced by the Let’s Talk! Podcast Collective as a collaborative effort between students, the Accessible Education and Disability Resources Department, and the PCC Multimedia Department. We air new episodes bi-weekly on our home website, our Spotify channel, and on XRAY 91.1 FM and 107.1 FM.